In response to the critical need for information on how the COVID-19 pandemic would impact newborns, in March 2020 researchers from Children’s Hospital of Philadelphia (CHOP) partnered with researchers at University of Florida and with the American Academy of Pediatrics to launch the National Registry for the Surveillance and Epidemiology of Perinatal COVID-19. This registry ultimately collected data from 242 birth centers across the United States and included more than 8,000 pregnant persons and their newborns.
In collaboration with perinatal investigators at the Centers for Disease Control and Prevention, the team has now analyzed data collected in 2020 and 2021, before the wide availability of vaccines, and found that newborns were infected with SARS-CoV-2 at variable rates and without apparent short-term effects. However, researchers also observed a higher-than-expected number of preterm births and maternal in-hospital deaths over this period.
The analysis, which was led by Dustin D. Flannery, DO, MSCE, and Karen M. Puopolo, MD, Ph.D., from CHOP and Mark L. Hudak, MD, from the University of Florida, was recently published in Pediatrics.
The analysis focused on maternal and newborn data for pregnant persons who tested positive for SARS-CoV-2 infection any time from two weeks before to 10 days after delivery between April 6, 2020 and March 19, 2021. The researchers assessed the incidence of newborn SARS-CoV-2 infection as well as complications among pregnant persons and newborns.
Of 7,524 pregnant persons who tested positive for SARS-CoV-2 during this period and had a liveborn infant, the majority were asymptomatic (78.1%), while 18.2% were symptomatic but not hospitalized specifically for COVID-19, 3.4% were hospitalized for COVID-19 treatment, and 0.2% died in the hospital of COVID-related complications.
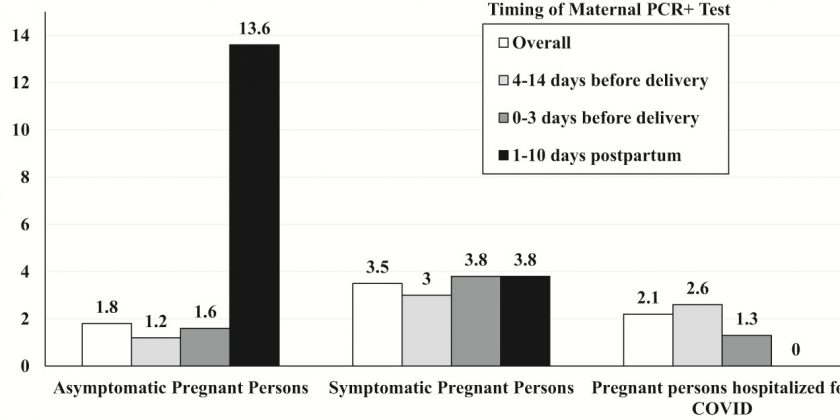
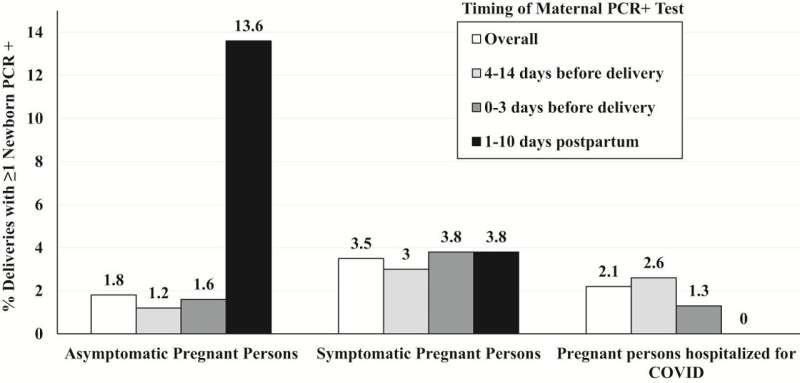
Among 7,648 newborns, 6,486 (84.8%) were tested for SARS-CoV-2, and 144 (2.2%) were positive; the highest rate of newborn infection was observed when mothers first tested positive in the immediate postpartum period.
No newborn deaths were attributable to SARS-CoV-2 infection. However, more babies who tested positive via PCR were born preterm compared than those who were negative (30.1% vs. 16.2%). Those with positive tests were more likely to be admitted to a NICU but were not more likely to need mechanical ventilation.
“Our findings provide strong rationale for mitigation measures, including maternal vaccination against SARS-CoV-2 infection, particularly with evidence of vaccine effectiveness to prevent severe disease among both pregnant persons and young infants,” said senior study author Karen M. Puopolo, MD, Ph.D., an attending neonatologist at Children’s Hospital of Philadelphia and Chief of the Section on Newborn Medicine at Pennsylvania Hospital. “It remains to be determined if newborn SARS-CoV-2 infection with past or future variants will have long-term consequences.”
More information:
Mark L. Hudak et al, Maternal and Newborn Hospital Outcomes of Perinatal SARS-CoV-2 Infection: A National Registry, Pediatrics (2023). DOI: 10.1542/peds.2022-059595
Journal information:
Pediatrics
Source: Read Full Article