Stephanie Santoro, MD, Director of Quality Improvement Research for the Down Syndrome Program within Mass General for Children and an assistant professor of Pediatrics at Harvard Medical School, was the lead author of a recent article in published in The Journal of Pediatrics titled “Health Surveillance in a Down Syndrome Specialty Clinic: Implementation of Electronic Health Record Integrations During the Coronavirus Disease 2019 Pandemic.”
She answered questions about her research in a short interview.
What was the question you set out to answer with this study?
As each primary care pediatrician typically cares for one to two patients with Down syndrome, the current care model involves the primary care physician providing health supervision for children with Down syndrome following the American Academy of Pediatrics’ (AAP) Clinical Report.
Studies show wide variation in adherence to the various recommended care elements in the AAP’s report, and we wanted to address gaps in routine recommended care for children with Down syndrome, through quality improvement during the coronavirus disease 2019 (COVID-19) pandemic.
We began this initiative within our subspecialty clinic for Down syndrome, the Massachusetts General Hospital Down Syndrome Program (MGH DSP), to attempt to improve health supervision. We based our approach on our previous work in another hospital system, which demonstrated that a combination of EHR tools using the same EHR system, Epic (Epic Systems Corp), improved adherence for patients with Down syndrome.
What methods or approach did you use?
Our main objective was to address gaps in routine recommended care for children with Down syndrome, through quality improvement during the coronavirus disease 2019 (COVID-19) pandemic.
To do this, we conducted a retrospective chart review of patients with Down syndrome. Records of visits to the Massachusetts General Hospital Down Syndrome Program were assessed for adherence to five components of the 2011 American Academy of Pediatrics (AAP) Clinical Report, “Health Supervision for Children with Down Syndrome.”
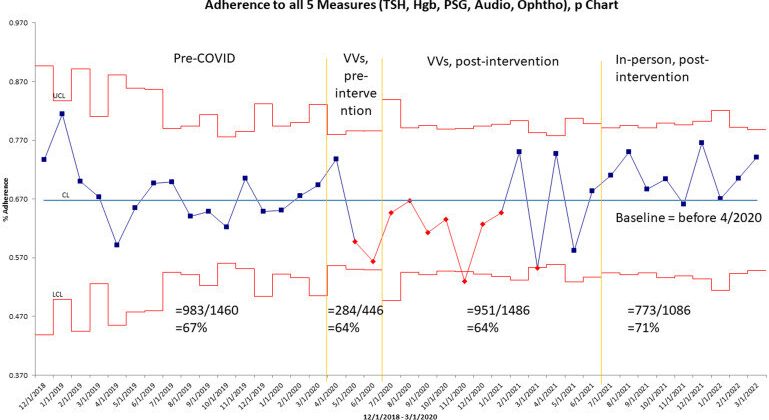
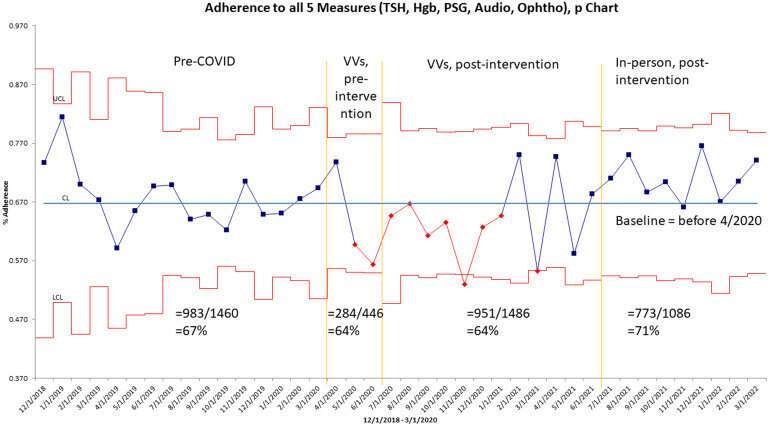
The impact of two of the major changes was analyzed using statistical process control charts. The first was a planned intervention of integrations to the electronic health record for routine health maintenance with age-based logic based on a diagnosis of Down syndrome, created and implemented in July 2020. The second major change was a natural disruption in care due to the COVID-19 pandemic, starting in March 2020.
Our approach was unique in that we studied adherence to health care guidelines during the COVID-19 pandemic. We integrated components directly into the health record.
What did you find?
From December 2018 to March 2022, total adherence to the five AAP guideline components was greater for follow-up visits compared with new patient visits (69% and 61%, respectively). Adherence to the audiology component decreased from 58% to 45%, while ophthalmology evaluation remained stable.
There was also improvement in adherence to thyroid-stimulating hormone, hemoglobin and sleep study components throughout the study.
What are the implications?
The COVID-19 pandemic influenced adherence to components of the AAP Health supervision for children with Down syndrome, but improvements in adherence coincided with implementation of our intervention and reopening after the COVID-19 pandemic.
What are the next steps?
We want to continue to study adherence after the COVID-19 pandemic and we want to work on improving adherence to hearing tests. Specifically, we want to study adherence outside of our Down Syndrome Program to assess adherence more broadly.
More information:
Stephanie L. Santoro et al, Health Surveillance in a Down Syndrome Specialty Clinic: Implementation of Electronic Health Record Integrations During the Coronavirus Disease 2019 Pandemic, The Journal of Pediatrics (2022). DOI: 10.1016/j.jpeds.2022.10.021
Journal information:
Journal of Pediatrics
Source: Read Full Article