In a recent study posted to the bioRxiv* preprint server, researchers demonstrated that the soluble P2X7 receptor is increased in severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) patients. They also showed that the elevated P2X7 receptors correlated with coronavirus disease 2019 (COVID-19) severity.
Inflammation is a well-coordinated response against viral or bacterial infection induced by the generation of pro-inflammatory cytokines. COVID-19 is characterized by the inflammatory response regulated by the stimulation of the nucleotide-binding oligomerization domain (NOD)- leucine-rich repeats (LRR)- and pyrin domain-containing protein 3 (NLRP3) inflammasome. The activated NLRP3 inflammasome leads to the release of interleukin-18 (IL-18) and IL-1β and pyroptotic cell apoptosis.
Of note, SARS-CoV-2 infection causes severe inflammation in the lungs, which leads to acute respiratory distress syndrome (ARDS), hypoxia, and pneumonia, all of which eventually results in COVID-19-related mortality.
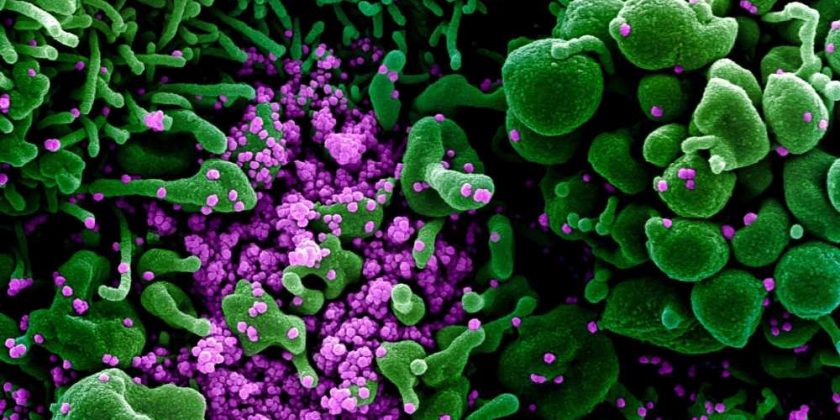
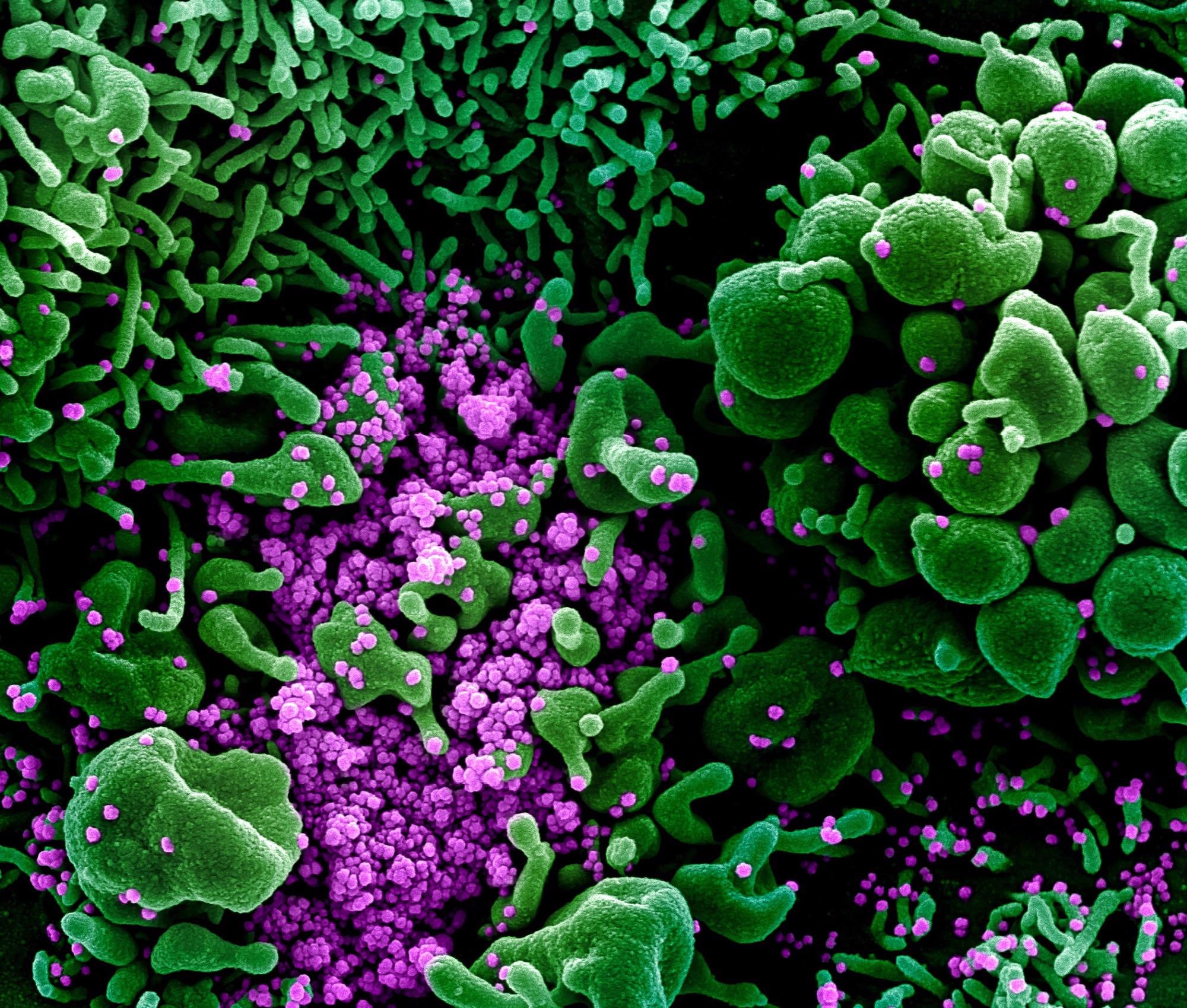 Study: Soluble P2X7 receptor is elevated in the plasma of COVID-19 patients and correlates with disease severity. Image Credit: NIAID
Study: Soluble P2X7 receptor is elevated in the plasma of COVID-19 patients and correlates with disease severity. Image Credit: NIAID
About the study
In the current study, the researchers evaluated the levels of various inflammatory markers in COVID-19 patients. They analyzed 208 plasma samples from SARS-CoV-2-infected individuals from the Murcia region of Southeast Spain during September 2020 and March 2021.
Further, samples from 69 subjects from the same geographical location without COVID-19 or other infection or inflammatory symptoms procured between 2016 and 2019 served as controls.
Findings and discussions
The results indicate that in the plasma of SARS-CoV-2-infected individuals, the acute phase C reactive protein (CRP) was increased beyond the standard threshold. Although procalcitonin (PCT) levels were only high in a few COVID-19 patients, ferritin levels were elevated in the majority.
As anticipated, IL-6 cytokine was increased in the plasma of SARS-CoV-2 patients compared to healthy controls. Further, in line with prior reports, IL-18, IL-1 receptor antagonist (IL-1 RA), and IL-15 were all elevated in the plasma of COVID-19 patients. Other chemokines or cytokines that have been shown to rise in SARS-CoV-2 patients, such as IL-2 and CCL2/monocyte chemoattractant protein-1 (MCP-1), were not enriched in the present cohort of COVID-19 patients relative to healthy subjects.
Soluble P2X7 receptor was substantially elevated in the plasma of COVID-19 patients compared to healthy participants. In contrast, additional pyroptosis markers such as gasdermin D (GSDMD), apoptosis-associated speck-like protein containing a CARD (ASC), and high mobility group box protein 1 (HMGB1) were not increased in SARS-CoV-2 patients relative to healthy subjects.
According to the COVID-19 severity, the levels of CRP in the plasma of SARS-CoV-2 patients rose dramatically. There were 39 severe, 128 moderate, and 41 mild COVID-19 cases in the study. Only the severe COVID-19 group exhibited a substantial increase in PCT levels. Ferritin levels were higher in the moderate and severe SARS-CoV-2 groups than in the mild group.
Plasma levels of IL-1RA and P2X7 receptors were considerably higher in COVID-19 patients throughout all severity categories compared to healthy subjects. The rise in P2X7 receptors in COVID-19 patients' plasma was age-independent as a rise across all age categories was identified. However, only in the 60-80-year group, there was a significant hike. In mild COVID-19 cases, IL-15 and IL-6 levels were not elevated, though they were considerably higher in moderate and severe SARS-CoV-2 cases. IL-18 was markedly elevated only in moderate COVID-19 patients.
The concentration of soluble P2X7 receptor, and the cytokines IL-15 and IL-6, was positively linked with CRP levels in the plasma. The positive association between the P2X7 receptor and CRP improved in the moderate and severe SARS-CoV-2 categories. In contrast, the link between IL-15 and IL-6 and CRP decreased in these categories. Both IL-18 and IL-1RA did not correlate with CRP in SARS-CoV-2 patients. Although ferritin was positively linked to CRP, ferritin demonstrated a weak association with the P2X7 receptor and did not correlate with IL-18. Further, the soluble P2X7 receptor positively correlated with various cytokines examined and demonstrated the best association with IL-18. These inferences indicate that the soluble P2X7 receptors increase with the severity of SARS-CoV-2 infection.
The addition of adenosine triphosphate (ATP) increased the P2X7 receptor concentration in the lipopolysaccharides (LPS)-treated peripheral blood mononuclear cells (PBMCs) supernatant. The ATP and LPS-addition also activated the NLRP3 inflammasome, indicated by the IL-1β release. In addition, the Pyrin inflammasome activation also led to the release of IL-1β and P2X7 receptors. This observation suggests that inflammasome-dependent caspase-1 and P2X7 receptor activation were connected to the P2X7 receptor shedding from human blood cells.
Conclusions
The study findings showed that the soluble P2X7 purinoceptor level was elevated in human plasma during COVID-19 in addition to the hike in IL-1RA, IL-18, and IL-6 receptors. While the increase in CRP concentration and COVID-19 severity is positively linked to the enhanced P2X7 receptor levels, it did not correlate with the IL-18 cytokine elevation. Furthermore, following inflammasome activation, the P2X7 receptor was detected in the supernatant of human peripheral blood mononuclear cells. These inferences imply that P2X7 receptor identification in the plasma might be a potential biomarker of SARS-CoV-2 severity.
*Important notice
bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Soluble P2X7 receptor is elevated in the plasma of COVID-19 patients and correlates with disease severity, Julio Garcia-Villalba, Laura Hurtado-Navarro, Alejandro Peñin-Franch, Cristina Molina-Lopez, Laura Martinez-Alarcon, Diego Angosto-Bazarra, Alberto Baroja-Mazo, Pablo Pelegrin, bioRxiv 2022.03.04.483019; doi: https://doi.org/10.1101/2022.03.04.483019, https://www.biorxiv.org/content/10.1101/2022.03.04.483019v1
Posted in: Medical Science News | Medical Research News | Disease/Infection News
Tags: Acute Respiratory Distress Syndrome, Adenosine, Adenosine Triphosphate, Apoptosis, Biomarker, Blood, CCL2, Cell, Chemokines, Coronavirus, Coronavirus Disease COVID-19, Cytokine, Cytokines, Hypoxia, Inflammasome, Inflammation, Interleukin, Leucine, Lungs, Monocyte, Mortality, Nucleotide, Pneumonia, Procalcitonin, Protein, Receptor, Respiratory, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Syndrome

Written by
Shanet Susan Alex
Shanet Susan Alex, a medical writer, based in Kerala, India, is a Doctor of Pharmacy graduate from Kerala University of Health Sciences. Her academic background is in clinical pharmacy and research, and she is passionate about medical writing. Shanet has published papers in the International Journal of Medical Science and Current Research (IJMSCR), the International Journal of Pharmacy (IJP), and the International Journal of Medical Science and Applied Research (IJMSAR). Apart from work, she enjoys listening to music and watching movies.
Source: Read Full Article