A new SARS-CoV-2 vaccine candidate, developed by giving a key protein’s gene a ride into the body while encased in a measles vaccine, has been shown to produce a strong immune response and prevent SARS-CoV-2 infection and lung disease in multiple animal studies.
Scientists attribute the vaccine candidate’s effectiveness to strategic production of the antigen to stimulate immunity: using a specific snippet of the coronavirus spike protein gene, and inserting it into a sweet spot in the measles vaccine genome to boost activation, or expression, of the gene that makes the protein.
Even with several vaccines already on the market, researchers say this candidate may have advantages worth exploring—especially related to the measles vaccine’s established safety, durability and high-efficacy profile.
“The measles vaccine has been used in children since the 1960s, and has a long history of safety for children and adults,” said Jianrong Li, senior author of the study and a professor of virology in The Ohio State University Department of Veterinary Biosciences.
“We also know the measles vaccine can produce long-term protection. The hope is that with the antigen inside, it can produce long-term protection against SARS-CoV-2. That would be a big advantage, because right now we don’t know how long protection will last with any vaccine platforms.”
The Ohio State Innovation Foundation has exclusively licensed the technology to Biological E. Limited (BE), a Hyderabad, India-based vaccine & pharmaceutical company.
The research is published online today in the journal Proceedings of the National Academy of Sciences.
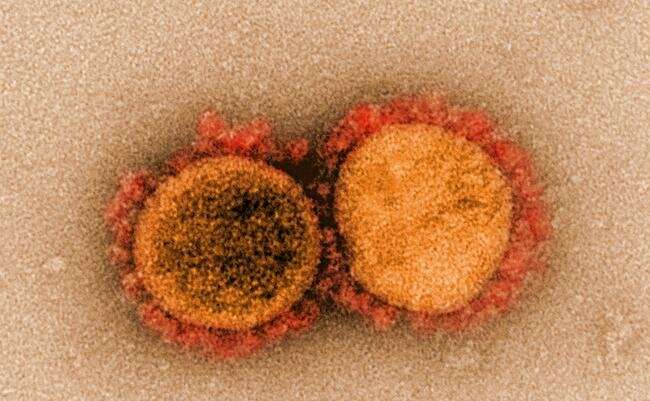
The coronavirus that causes COVID-19 uses the spike protein on its surface to bind to its target cells in the nose and lungs, where it makes copies of itself and releases them to infect other cells. Like all vaccines, this candidate initiates the production of antibodies that recognize the new protein as foreign, training the immune system to attack and neutralize the spike protein if SARS-CoV-2 ever enters the body.
Li created the COVID-19 vaccine using a live attenuated measles virus as a vehicle with colleagues Mijia Lu, a postdoctoral researcher in Li’s laboratory and first author on the paper, and co-authors Stefan Niewiesk, Ohio State professor of veterinary biosciences, and Mark Peeples, professor of pediatrics at Ohio State and a researcher at Nationwide Children’s Hospital in Columbus.
For this work, the researchers tested seven versions of the spike protein to find the most effective antigen. They landed on a stabilized “prefusion” version of the protein—the shape the protein is in before it infects a cell.
The scientists inserted the prefusion spike protein gene containing manufacturing instructions into a segment of the measles vaccine genome to generate high expression of the protein, reasoning that the more SARS-CoV-2 spike protein produced, the better the immune response.
The team tested the vaccine candidate in several animal models to gauge its effectiveness, and found that the vaccine induced high levels of neutralizing antibodies against SARS-CoV-2 in all of the animals.
Some may think most humans’ immunity to measles, thanks to decades of widespread vaccination, would render its status as a coronavirus vaccine vehicle useless. To quell those concerns, researchers gave cotton rats a measles vaccine and showed that a second immunization with the measles-based SARS-CoV-2 vaccine candidate could induce a strong neutralizing antibody response to the coronavirus.
Genetically modified mice produced helper T cells—a type of white blood cell—in response to the vaccine, another important way the body fights infection, and severe disease in particular.
“The orientation of T helper cells induced by a vaccine is an important predictor of protection, and this vaccine mainly induces Th1 cells, which enhances the safety and efficacy of the vaccine,” said co-author Amit Kapoor, associate professor of pediatrics at Ohio State and a researcher at Nationwide Children’s Hospital.
Golden Syrian hamsters, which are susceptible to contracting COVID-19, received the vaccine and were then injected with the coronavirus. The vaccinated hamsters were protected from lung infection and other sickness symptoms indicated through weight loss.
“When we looked at the amount of neutralizing antibody induced in the hamster, it was actually higher than from people who had been infected with COVID, suggesting the vaccine may be better than SARS-CoV-2 infection in inducing protective immunity. That was our goal,” Peeples said.
The researchers have confidence in the platform not only because the measles vaccine is safe, effective and affordable to produce, but because several experimental measles-based vaccines against other viruses are in development. A vaccine against chikungunya virus, spread by mosquitos, has been shown to be safe, well-tolerated and good at provoking an immune response in a Phase 2 clinical trial.
And even with a variety of COVID-19 vaccines now available in the United States and other countries, there is still a lot to learn about which are the safest and most effective for specific populations, such as children and pregnant women, and which vaccines are the most economical to produce.
“We can make vaccines much more quickly now than in the past. But if we had to do it the traditional way this time, we wouldn’t have a vaccine protecting us in this short amount of time,” Niewiesk said. “The mRNA vaccines in use now were made in record time. And they protect against disease and are safe. Although not quite as fast, we were able to make this vaccine much more quickly than the original measles vaccine.
Source: Read Full Article
