Our immune systems react most strongly to the viral strains we encountered in our childhoods. Scientists call this original antigenic sin (OAS)—the body’s first blush with a virus like influenza or COVID being the “original sin” that forever biases its immune response against newer strains. According to the OAS theory, no matter how many flu vaccines or COVID boosters we receive, our bodies would stubbornly insist on churning out tired antibodies against a bygone strain of a virus.
Now, a new study provides some of the cleanest evidence to date for when OAS does and does not happen, clarifying how this otherwise hazy phenomenon actually works when studied in the laboratory. The findings, published in Nature, may have far-reaching implications for the development of influenza and COVID vaccines.
“Our goal was to understand the basic principles that underlie OAS so that researchers making these vaccines can keep the potential effects in mind,” says Rockefeller’s Gabriel D. Victora. “With a novel technique, we lay out the basics of how OAS should be looked at from an experimental perspective and answer a question we believe to be key to vaccine development.”
Antigenic sin
OAS was initially described in the 1950s by Thomas Francis Jr., a legendary virologist who isolated the first human influenza strain in the U.S. The son of a Presbyterian minister, Francis chose decidedly religious terminology to capture his frustration with the immune system’s tendency to imprint on the first antigen it encounters, even to its own detriment.
“Francis realized that you could figure out someone’s age by looking at their antibodies against flu,” Victora says. “People’s strongest antibodies were usually to the strains circulating when they were young.”
“Love it or hate it, the term has stuck and become a staple in conversations about viral vaccination.”
If OAS were strictly true, it would be difficult for a vaccine program to overcome the body’s resistance to change. Upon exposure to a new flu strain via seasonal vaccines, the body would just repeatedly reuse its original cohort of B cells and to suppress the formation of new ones. “According to the OAS idea, your body wouldn’t be able to develop new immune responses to evolving variants of a virus, because it would be addicted to the first strain you encountered,” Victora says.
Despite half a century of epidemiological evidence of this frustrating phenomenon, however, the precise extent of OAS proved difficult to measure in a laboratory setting. “It was not easy to generate good experimental data on OAS,” Victora says. “Prior experiments have given discrepant results—sometimes researchers see it, and sometimes they don’t.”
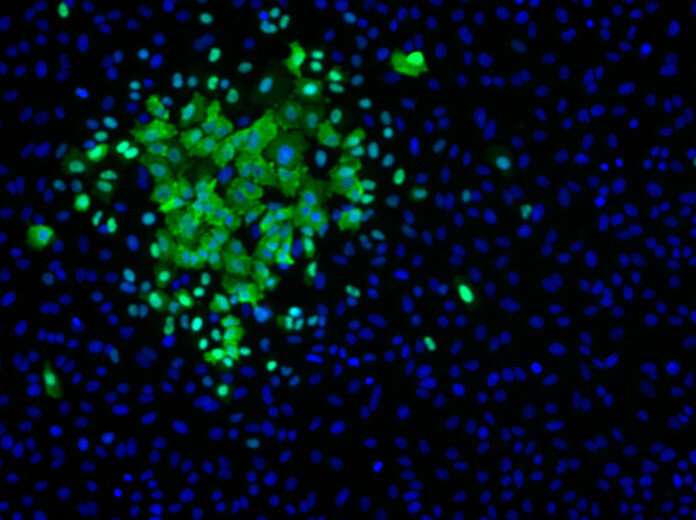
In an attempt to better understand OAS and its impacts on seasonal vaccines and booster shots, Victora and colleagues developed molecular fate-mapping, a technique which allowed the team to clearly distinguish old antibodies from new ones in serum. They then exposed mice to one immunization after another, while tracking the progress of every last antibody.
The findings confirmed, experimentally, that, when the antigen was kept the same, the mice were “addicted” to the first B cells they produced, and that these B cells were preventing the formation of new B cells to respond to novel threats.
“We estimate that the mice would have made 55-fold more new antibodies were their old antibodies not around to suppress the formation of new ones,” Victora says.
Antigenic redemption
On the surface, these findings would appear to imply that seasonal shots and boosters are exercises in futility. The body is doomed to produce B cells attuned to everyone’s first COVID or flu exposure, ignoring and even suppressing inoculations against new strains.
“But there’s a twist,” Victora says. If the booster shot contains an antigen sufficiently different from the original antigen, OAS steps into the sidelines. Indeed, Victora and colleagues demonstrate in mice infected with a variety of influenza virus and SARS-CoV-2 strains that once two antigens are even a few amino acids apart, that 55-fold deficit falls to a manageable three-fold.
“This work provides a basic understanding of the way B cells respond to a series of booster vaccines and underscores the ingenuity and adaptability of the immune system,” says first author Ariën Schiepers, a graduate student in Victora’s lab and the first author on the paper. “When boosting with a variant antigen, we begin to see new, variant-specific antibodies that enable the subversion of OAS.”
Although the findings are confined to mice, Victora suspects the message may be universal. Should the trend hold in humans, the team’s findings would imply that boosting against a new strain of SARS-CoV-2 will bear the most fruit if the new strain is sufficiently different from the one covered by the previous vaccine (which, by the way, is clearly the case for the case bivalent COVID vaccines currently in clinical use).
“It may well be a matter of waiting to update vaccines until the virus is sufficiently divergent. That would be just the right time to develop a booster.”
More information:
Ariën Schiepers et al, Molecular fate-mapping of serum antibody responses to repeat immunization, Nature (2023). DOI: 10.1038/s41586-023-05715-3
Journal information:
Nature
Source: Read Full Article
