Performing endovascular thrombectomy in patients with an ischemic stroke having a large ischemic core has been found to be beneficial in a major international trial, which is expected to lead to a change in clinical practice and the way in which systems of stroke care are organized.
The results of the SELECT2 trial, which was conducted in sites in the United States, Canada, Europe, Australia, and New Zealand, showed that endovascular thrombectomy plus medical care resulted in better clinical outcomes than medical care alone in patients with a large ischemic core who presented within 24 hours after the time they were last known to be well.
The results of the SELECT2 trial were presented today by Amrou Sarraj, MD, at the International Stroke Conference (ISC) 2023 in Dallas, Texas. Sarraj is professor of neurology at University Hospitals Cleveland Medical Center–Case Western Reserve University in Ohio.
The study was also simultaneously published online in the New England Journal of Medicine.
A similar trial conducted in China, the ANGEL-ASPECT trial, was also presented at the same ISC session and showed very similar results.
These two trials add to another Japanese study reported last year, the RESCUE-JAPAN LIMIT trial, also showing benefit of thrombectomy in patients with large core strokes.
Sarraj concluded that the results of these three trials together “unequivocally demonstrate the benefit of endovascular thrombectomy in patients with large ischemic core.”
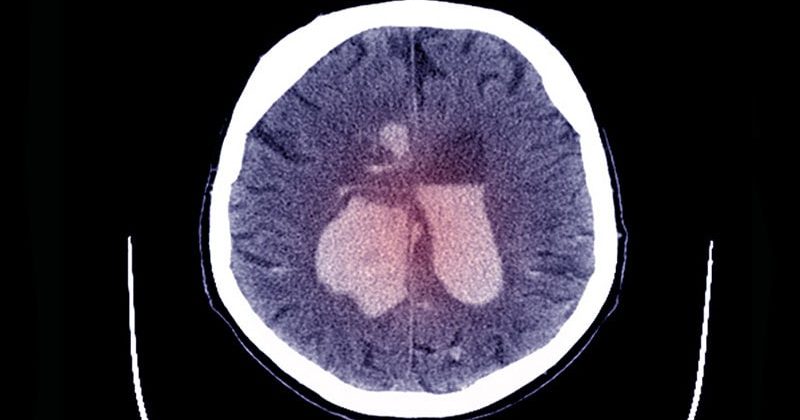
Approximately 20% of large-vessel occlusion strokes have a large core, but these patients have not been considered candidates for endovascular thrombectomy because of concerns about potential reperfusion injury in necrotic brain tissue, resulting in an increased risk of hemorrhage, edema, disability, and death.
This has resulted in uncertainty about how to manage these patients with a core infarct, Sarraj noted.
The SELECT2 trial involved patients with stroke as a result of occlusion of the internal carotid artery or the first segment of the middle cerebral artery. Patients had a large ischemic-core volume, defined as an ASPECTS (Alberta Stroke Program Early Computed Tomography Score) of 3 to 5 or a core volume of at least 50 mL on imaging. They were randomly assigned to endovascular thrombectomy plus medical care or to medical care alone.
The trial was aiming to enroll 560 patients but was stopped early for efficacy after 178 patients had been assigned to the thrombectomy group and 174 to the medical-care group.
The primary outcome — the generalized odds ratio for a shift in the distribution of modified Rankin scale scores toward better outcomes in favor of thrombectomy was 1.51 (P < .001).
“This translates into a 60% probability of achieving a better functional outcome in patients receiving thrombectomy, with a number needed to treat of 5. That means 5 patients need to be treated with thrombectomy for one to achieve a better functional outcome,” Sarraj stated.
The secondary outcome of functional independence at 90 days (a score on the modified Rankin scale of 0-2) occurred in 20% of the patients in the thrombectomy group and 7% in the medical-care group (relative risk, 2.97), with a number needed to treat of 7.
Independent ambulation (a score on the modified Rankin Scale of 0-3) at 90 days occurred in 37.9% of the patients in the thrombectomy group and in 18.7% of the patients in the medical-care group (relative risk, 2.06), with a number needed to treat of 5.
Mortality was similar in the two groups.
The results for other secondary outcomes were generally in the same direction as those of the primary analysis, with the possible exception of early neurologic improvement, the authors report.
The incidence of symptomatic intracranial hemorrhage was low in both trial groups, occurring in one patient in the thrombectomy group and two in the medical-care group.
The investigators point out that previous studies have reported rates of symptomatic intracranial hemorrhage in patients with large ischemic-core lesions that are higher than those in this trial. “Therefore, the low percentage of patients with symptomatic intracranial hemorrhage observed in both trial groups was unexpected.”
Approximately 20% of the patients in the thrombectomy group had complications associated with the procedure. In the thrombectomy group, arterial access-site complications occurred in 5 patients, dissection in 10, cerebral-vessel perforation in 7, and transient vasospasm in 11.
Early neurologic worsening, defined as an increase of 4 or more points on the National Institutes of Health Stroke Scale (NIHSS), occurred in 24.7% in the thrombectomy group and in 15.5% in the medical-care group (relative risk, 1.59).
In a post-hoc analysis, “from which no conclusions can be drawn,” the authors report, early neurologic worsening was associated with worse functional outcomes at 90 days, and patients who had neurologic worsening had larger ischemic-core lesions at baseline (median volume, 107 mL) vs 77 mL among patients without neurologic worsening.
They note that a potential cause of deterioration in some of these patients was brain edema associated with reperfusion. However, they emphasize that overall, endovascular thrombectomy was associated with better outcomes than medical care alone.
“Two thirds of patients had core infarct sizes more than 70 mL, and one third of patients had core infarct sized of more than 100 mL, but even in patients with large and very large core volumes, thrombectomy was superior to medical care alone,” Sarraj said.
This Will “Change Practice”
Commenting on the study for theheart.org | Medscape Cardiology, ISC 2023 chair Tudor Jovin, MD, Cooper Neurological Institute, Cherry Hill, New Jersey, said: “This trial shows that even patients with a large core infarct who we would not have treated with thrombectomy in the past, actually do benefit from this procedure. And the surprise is that the benefit is nearly to the same extent as that in patients with smaller core infarcts. That is going to change practice.”
Jovin said that these results should not only change the selection of patients for thrombectomy, but they should also change systems of care. “Because the systems of care now are based around excluding these patients with large infarcts. We won’t need to do that in future.”
He elaborated: “I think imaging has held us back to be honest. We can exclude hemorrhage with a plain CT scan. Then after this, the biggest piece of information we need from imaging is the size of the infarct. We were concerned that we might hurt the patient if the infarct was large. Outside hospitals had to do advanced imaging before deciding whether to transfer patients for thrombectomy. These are all sources of delays.
“I am very pleased to see these results and I hope to see a much more simplified triage of patients that will be more liberal to patients with the large infarcts,” he added.
Also commenting for theheart.org | Medscape Cardiology, Joseph Broderick, MD, professor of neurology and director of the Neuroscience Institute at the University of Cincinnati, said the results were “robust and important.”
He said the results of the SELECT2 trial, along with the other two similar trials, “will change practice and extend endovascular therapy to more patients with severe strokes.”
But Broderick believes imaging will still be necessary to exclude patients with ASPECTS scores of 0-2, who were not included in these trials. “These are patients who have very large areas of clear hypodensity on the baseline image (brain already dying or dead). These patients do not benefit from reperfusion with lytic drugs or endovascular therapy,” he noted.
“Welcome News”
In an NEJM editorial accompanying the publication of the two new studies, Pierre Fayad, MD, University of Nebraska Medical Center, Omaha, points out that all three trials of thrombectomy in patients with large core infarct strokes “showed remarkably similar results” despite differences in design, patient selection, thrombolytic treatment and dose, geographic location, and imaging criteria.
“Together, the trials provide reassuring information from more than a thousand patients with large ischemic strokes in different medical systems that will probably lead to changes in patterns of care delivery.”
Fayad says it is reasonable to suggest that endovascular thrombectomy be offered to patients with large strokes if they arrive in a timely fashion at a center that is capable of performing the procedure, and if the patients have an ASPECTS value of 3-5 or an ischemic-core volume of 50 mL or greater.
Higher rates of good outcomes may be anticipated if this treatment is performed, despite increased risks of symptomatic hemorrhage, edema, neurologic worsening, and hemicraniectomy, he notes.
“Patients and families should be made aware of the limitations of treatment and the anticipated residual neurologic deficits resulting from the large infarction. The improved chance of independent walking and the ability to perform other daily activities in patients with the most severe strokes is welcome news for patients and for the field of stroke treatment,” he concludes.
The SELECT2 trial was supported by an investigator-initiated grant from Stryker Neurovascular to University Hospitals Cleveland Medical Center and the University of Texas McGovern Medical School.
International Stroke Conference (ISC) 2023: Presentation LB21. Presented February 10, 2023.
N Eng J Med. Published online February 10, 2023. Full text, Editorial
For more from theheart.org | Medscape Cardiology, follow us on Twitter and Facebook
Source: Read Full Article