A significant amount of genetic risk for asthma is likely mediated through altered gene expression within the airway epithelium. That is the conclusion of a National Jewish Health-led study to identify genetic variants that cause asthma by altering the function of airway cells. The team’s paper published March 28, 2022, in the journal Nature Communications.
“This work will help us identify targetable pathways to intervene for asthma, to stop mucus hypersecretion or type 2 airway inflammation, an allergic response that can exacerbate asthma,” said Max A. Seibold, Ph.D., professor of Pediatrics in the National Jewish Health Center for Genes, Environment and Health and senior author of the paper. “One of the banes of human existence is mucus, which plays a role in so many health conditions, everything from the common cold, to COVID, to chronic lung diseases like asthma and COPD. The more we know about what causes it, the better equipped we will be to develop impactful treatments.”
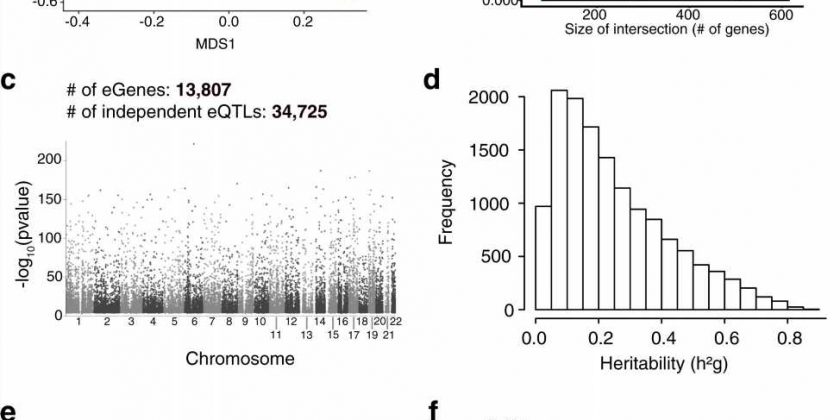
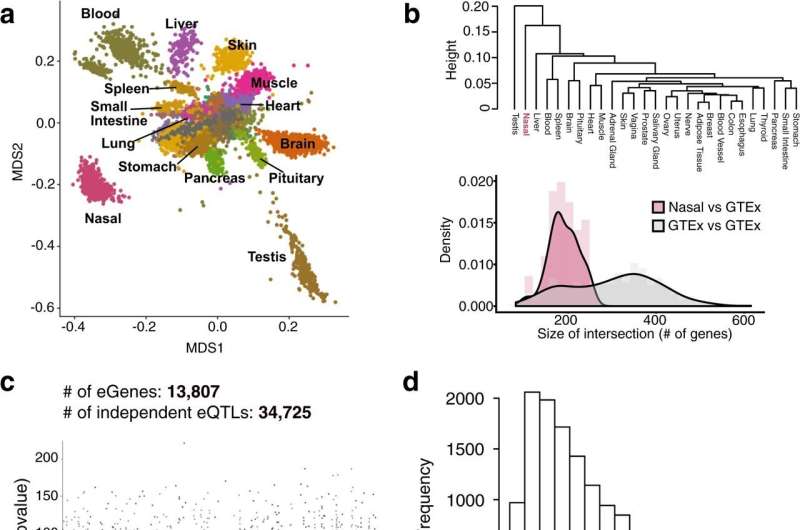
For the study, the team performed the first airway transcriptome-wide association study (TWAS) for childhood and adult onset asthma. The first step in a TWAS study is to build models that will allow prediction of how a person’s genes will function in a particular tissue, based solely on their genetic profile. Dr. Seibold and colleagues leveraged nasal airway samples and genetic data from a cohort of 700 children in Puerto Rico, who either were in good health or had asthma, to build these models for airway tissue.
The team then applied these models to genetic data from over 300,000 participants in the UK Biobank study, a large-scale biomedical database and research resource. This allowed them to test whether genetically altered function of airway genes is associated with asthma risk. The study data found over a third of identified genetic risk factors for asthma may confer their risk through alteration of the cells that line the airways (i.e. airway epithelium).
In particular, the researchers found genetic changes in a gene that forms the structure of mucus (MUC5AC), and another gene (FOXA3) that directs the production of mucus secretory cells. This is one of the first times anyone has found genetic variants that influence asthma risk through the alteration of mucus secretory function. The team also found that some of the key genes in the type 2 inflammatory pathway have genetic changes that increase their level of expression in the airway, increasing asthma risk.
“This study demonstrates how obtaining additional data on the expression of genes from participants in genome-wide association studies can shed light on their biological functions. It also shows that some genes may be expressed differently in different tissues,” said James P. Kiley, Ph.D., director of the National Heart, Lung, and Blood Institute (NHLBI)’s Division of Lung Diseases. “Research like this moves us one step closer to developing personalized medicine treatments for asthma and other common diseases.”
Source: Read Full Article