Although national COVID mortality disparities declined in 2021, this decrease was largely explained by increases in mortality among White individuals and the shifting geography of the pandemic from urban to rural areas rather than decreases in mortality among non-Hispanic Black and Hispanic individuals.
The racial disparities in COVID-19 deaths became a defining part of the first year of the pandemic in the United States, prompting national efforts to reduce this disproportionate toll among Black and Hispanic communities through vaccination drives and other outreach when COVID vaccines became available in 2021.
Following these efforts, federal officials and the media touted major reductions in disparities in COVID mortality rates during the delta and omicron waves in the second year of the pandemic, but a new study led by Boston University School of Public Health (BUSPH) shows that the declines in these disparities do not reflect substantial improvements in population health to the extent previously thought.
Published in the journal JAMA Network Open, the study found that disparities in US COVID death rates between Black and White adults narrowed substantially from the first to the second year of the pandemic, from 339 deaths to 45 deaths per 100,000 people in 2021, after accounting for age.
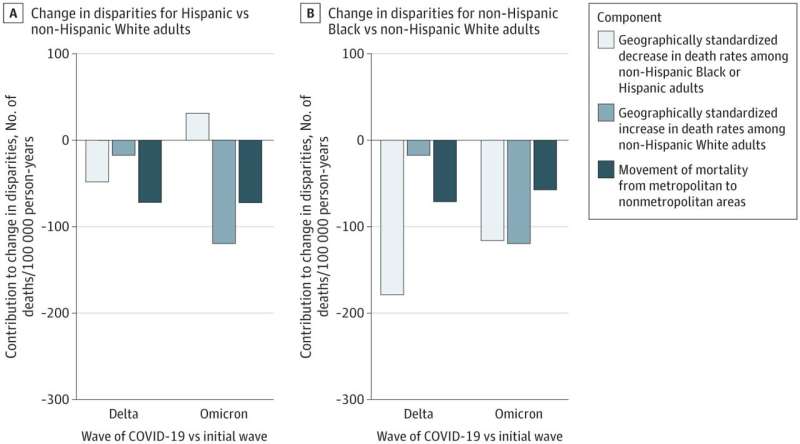
But this sharp decline mostly resulted from an increase in COVID deaths among White people, as well as a geographical shift in mortality from large, urban cities to rural and smaller metropolitan areas, rather than from decreases in deaths among the Black population.
Similarly, Hispanic-White disparities in deaths shrunk from 172 deaths to 12 deaths, and this decline was entirely due to increases in COVID deaths among White and rural populations.
Furthermore, while the findings showed that national COVID death rates for Black, Hispanic, and Asian populations did decrease by 2021, the death rates among these groups increased in rural areas in 2021 and exceeded White death rates.
This geographical shift in US COVID mortality and continued high death rates among racial and ethnic minority populations suggest that declarations of COVID-related racial equity achievements may be coming too soon. As the Biden administration prepares to lift the COVID public health emergency on May 11, much more work still needs to be done to address this burden among all populations.
“Contrary to popular media narratives, our findings indicate that decreases in racial and ethnic disparities in COVID were mostly explained by increases in mortality for White adults and changes in pandemic geography rather than decreases in Black and Hispanic mortality,” says study corresponding author Dr. Andrew Stokes, assistant professor of global health at BUSPH. “This suggests that it may be premature to celebrate reductions in disparities because they did not largely represent reductions in mortality.”
For the study, Dr. Stokes and colleagues utilized national data to examine COVID-related deaths among nearly one million US adults 25 and older from the initial wave of the pandemic in March 2020 to the Delta and Omicron waves through February 2022. The team examined these deaths by race and ethnicity across metropolitan and nonmetropolitan areas and developed an innovative mathematical framework to identify the factors contributing to the decline in disparities.
Through this framework, the researchers estimated that the rise in COVID deaths in rural areas—which increased from five percent of all rural deaths in 2020 to about 22 percent of all rural deaths by March 2022—and the increase in mortality among the White population explained about 60 percent of the decline in disparities, and the remainder was due to the national decline in deaths among the Black population.
The team also observed concerning trends among the American Indian/Alaska Native (AIAN) population. COVID deaths for this group appeared to increase at the national level during the Delta and Omicron waves, in both urban and rural areas.
Several social, political, geographical, and structural factors may contribute to these shifts in COVID mortality rates. Vaccination and booster rates play a central role—the researchers say the politicized nature of vaccines likely led to lower uptake of the primary series among White and rural people, and Black, Hispanic, and AIAN people have received substantially fewer boosters than White people. Rural residents also experience greater rates of chronic diseases, a risk factor for severe COVID infection, as well as greater difficulty accessing care.
“The social and structural determinants of health that have contributed to the racial and ethnic disparities in mortality observed during the pandemic remain largely unaddressed,” says study first author Dielle Lundberg, research assistant at BUSPH and doctoral student at the University of Washington School of Public Health. “Ongoing work to address these determinants of health, along with increased efforts to ensure booster uptake in rural communities, especially among older adults, are still urgently needed.”
The researchers also urge community investments and policy changes that will remove social and economic barriers largely driven by structural racism, increase access to community resources, and close the racial health equity gap.
“These results underscore COVID’s ongoing toll, even in the vaccinated era,” says study co-author Dr. Elizabeth Wrigley-Field, assistant professor of sociology at the University of Minnesota College of Liberal Arts. “Full protection can’t rest only on vaccination or other choices that individuals can make—it also means social policies like paid sick leave, new standards for indoor air quality in workplaces and schools, and expanding and diversifying the healthcare workforce, especially in rural areas.”
More information:
Dielle J. Lundberg et al, COVID-19 Mortality by Race and Ethnicity in US Metropolitan and Nonmetropolitan Areas, March 2020 to February 2022, JAMA Network Open (2023). DOI: 10.1001/jamanetworkopen.2023.11098
Journal information:
JAMA Network Open
Source: Read Full Article
