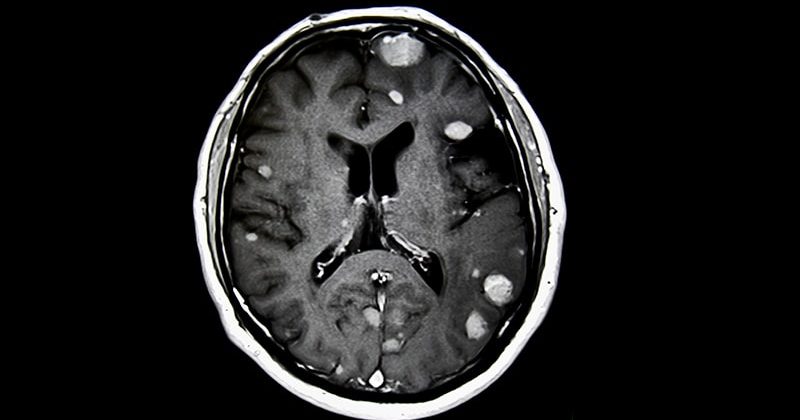
For patients with up to 10 brain metastases from small cell lung cancer (SCLC), stereotactic radiosurgery was associated with less cognitive impairment than whole-brain radiation therapy (WBRT) without compromising overall survival, results of the randomized ENCEPHALON (ARO 2018-9) trial suggest.
Among 56 patients with one to 10 SCLC brain metastases, 24% of those who received WBRT demonstrated significant declines in memory function 3 months after treatment, compared with 7% of patients whose metastases were treated with stereotactic radiosurgery alone. Preliminary data showed no significant differences in overall survival between the treatment groups at 6 months of follow-up, Denise Bernhardt, MD, from the Technical University of Munich, Germany, reported at the American Society of Radiation Oncology (ASTRO) annual meeting.
“We propose stereotactic radiosurgery should be an option for patients with up to 10 brain metastases in small cell lung cancer,” Bernhardt said during her presentation.
Vinai Gondi, MD, who was not involved in the study, told Medscape Medical News that the primary results from the trial — while limited by the study’s small size and missing data — are notable.
Patients with brain metastases from most cancer types typically receive stereotactic radiosurgery but WBRT has remained the standard of care to control brain metastases among patients with SCLC.
“This is the first prospective trial of radiosurgery vs whole-brain radiotherapy for small cell lung cancer brain metastases, and it’s important to recognize how important this is,” said Gondi, director of Radiation Oncology and codirector of the Brain Tumor Center at Northwestern Medicine Cancer Center, Warrenville, Illinois.
Prior trials that have asked the same question did not include SCLC because many of those patients received prophylactic cranial irradiation, Gondi explained. Prophylactic cranial irradiation, however, has been on the decline among patients with brain metastases from SCLC, following a 2017 study from Japan showing no difference in survival among those who received the therapy and those followed with observation as well as evidence demonstrating significant toxicities associated with the technique.
Now “with the declining use of prophylactic cranial irradiation, the emergence of brain metastases is increasing significantly in volume in the small cell lung cancer population,” said Gondi, who is principal investigator on a phase 3 trial exploring stereotactic radiosurgery vs WBRT in a similar patient population.
In a previous retrospective trial, Bernhardt and colleagues found that first-line stereotactic radiosurgery did not compromise survival compared with WBRT, but patients receiving stereotactic radiosurgery did have a higher risk for intracranial failure.
In the current study, the investigators compared the neurocognitive responses in patients with brain metastases from SCLC treated with stereotactic radiosurgery or WBRT.
Enrolled patients had histologically confirmed extensive disease with up to 10 metastatic brain lesions and had not previously received either therapeutic or prophylactic brain irradiation. After stratifying patients by synchronous vs metachronous disease, 56 patients were randomly assigned to either WBRT, at a total dose of 30 Gy delivered in 10 fractions, or to stereotactic radiosurgery with 20 Gy, 18 Gy, or fractionated stereotactic radiosurgery with 30 Gy in 5 Gy fractions for lesions larger than 3 cm.
The primary endpoint was neurocognition after radiation therapy as defined by a decline from baseline of at least five points on the Hopkins Verbal Learning Test-Revised (HVLT-R) total recall subscale at 3 months. Secondary endpoints included survival outcomes, additional neurocognitive assessments of motor skills, executive function, attention, memory, and processing as well as quality-of-life measures.
The investigators expected a high rate of study dropout and planned their statistical analysis accordingly, using a method for estimating the likely values of missing data based on observed data.
Among 26 patients who eventually underwent stereotactic radiosurgery, 18 did not meet the primary endpoint and two (7%) demonstrated declines on the HVLT-R subscale of five or more points. Data for the remaining six patients were missing.
Among the 25 who underwent WBRT, 13 did not meet the primary endpoint and six (24%) demonstrated declines of at least five points. Data for six of the remaining patients were missing.
Although more patients in the WBRT arm had significant declines in neurocognitive function, the difference between the groups was not significant, due to the high proportion of study dropouts — approximately one fourth of patients in each arm. But the analysis suggested that the neuroprotective effect of stereotactic radiosurgery was notable, Bernhardt said.
At 6 months, the team also found no significant difference in the survival probability between the treatment groups (P = .36). The median time to death was 124 days among patients who received stereotactic radiosurgery and 131 days among patients who received WBRT.
Gondi said the data from ENCEPHALON, while promising, need to be carefully scrutinized because of the small sample sizes and the possibility for unintended bias.
ARO 2018-9 is an investigator-initiated trial funded by Accuray Inc. Bernhardt disclosed consulting actives, fees, travel expenses, and research funding from Accuray and others. Gondi disclosed honoraria from UpToDate.
American Society of Radiation Oncology (ASTRO) 2023 Annual Meeting. Abstract LBA07. Presented October 1, 2023.
Neil Osterweil, an award-winning medical journalist, is a long-standing and frequent contributor to Medscape.
For more news, follow Medscape on Facebook, X (formerly known as Twitter), Instagram, and YouTube.
Source: Read Full Article