Ponatinib, a potent third-generation tyrosine kinase inhibitor (TKI), showed superior efficacy and comparable safety vs the first-generation TKI imatinib in patients with newly diagnosed Philadelphia chromosome-positive acute lymphoblastic leukemia (PH+ALL).
The agents were evaluated in the randomized, open-label, phase 3 PhALLCON study, the first head-to-head comparison of ponatinib and imatinib in combination with reduced-intensity chemotherapy in the Ph+ALL population.
Overall, patients in the ponatinib arm experienced a significantly higher minimal residual disease (MRD)-negative complete response rate as well as deeper and more durable responses compared with those in the imatinib arm, the investigators reported.
The findings were presented during American Society of Clinical Oncology (ASCO) virtual plenary session on February 15.
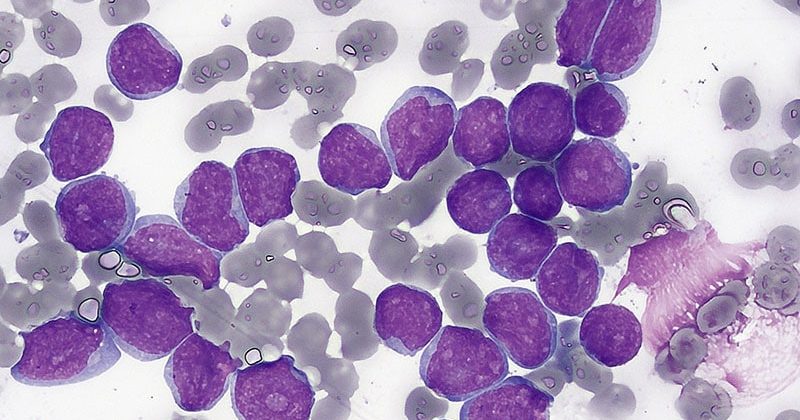
In adults with ALL, Ph+ disease is the most frequent genetic subtype, accounting for about one third of cases. The current standard of care for newly diagnosed Ph+ALL, also known as BCR-ABL-1-positive ALL, is BCR-ABL1 TKIs in combination with chemotherapy or steroids. However, when treated with first- or second-generation TKIs, patients eventually progress due to the emergence of treatment resistance.
Before the advent of TKI therapies, Ph+ALL had a very poor prognosis, but the development of imatinib in 2001 was transformative, said Marlise R. Luskin, MD, a senior physician at Dana-Farber Cancer Institute, Boston, Massachusetts, in the ASCO plenary session, exploring the state of the science.
Added to “backbone” chemotherapy regimens, imatinib improved complete response rates, increased eligibility for stem cell transplantation, and improved overall survival. Second-generation TKIs, including dasatinib and nilotinib further improved outcomes, said Luskin, also assistant professor at Harvard Medical School, Boston, Massachusetts.
More recently, ponatinib has emerged as a promising treatment given its unique action against the ABLA1 T315I KD mutation present in about 75% of cases that relapse as well as the findings of improved MRD-negative complete response rates and event-free survival in retrospective studies, Luskin said.
The PhALLCON study was designed to further investigate promising results seen in retrospective studies of ponatinib.
To assess ponatinib vs imatinib, patients were enrolled and randomized two to one to receive either a 30 mg once-daily starting dose of ponatinib or a once-daily 600 mg dose of imatinib plus reduced-intensity chemotherapy. After cycle 20, patients received single agent ponatinib or imatinib until disease progression or unacceptable toxicity.
Of the 245 enrolled, 78 remained on treatment at the August 2022 data cutoff, including 42% of those in the ponatinib arm and 12% in the imatinib arm. The most common reasons for discontinuation included hematopoietic stem cell transplantation (31% for ponatinib and 37% for imatinib), adverse events (12% in both arms), and lack of efficacy (7% and 26%, respectively).
At median follow-up of 20 months among 164 patients in the ponatinib arm and 18 months among 81 patients in the imatinib arm, the MRD-negative complete response rates were 34.4% and 16.7%, respectively, said first author Elias J. Jabbour, MD, a professor of medicine at the University of Texas MD Anderson Cancer Center, Houston, Texas.
A trend toward improved event-free survival was also observed in the ponatinib arm, but the data were not mature at the time of the analysis, Jabbour noted.
The two treatments showed comparable safety. Treatment-emergent adverse event rates of any grade and of grade 3 or higher were similar in the two study arms. Arterial occlusive events were infrequent and were also similar between the arms.
“Taken together, for this patient population, the efficacy and safety results demonstrate a favorable risk-benefit assessment for ponatinib, which should be considered a standard of care for frontline therapy in patents with newly diagnosed Ph+ALL,” Jabbour said.
Although the PhALLCON findings are encouraging, invited discussant Anjali S. Advani, MD, of the Cleveland Clinic in Ohio, noted some study “pitfalls and caveats,” including the generally younger age and low incidence of cardiovascular risk factors in the study population, which raises questions about the ability to extrapolate the findings to “the larger population, which may be older and have more comorbidities.”
Advani also said that the ponatinib vs imatinib comparison is a reasonable one, but that most clinicians are now using dasatinib, so “it would have been nice to have this comparison.”
Additionally, “the landscape is now changing with the use of blinatumomab plus TKIs — either dasatinib or ponatinib — in the upfront setting.”
“There is data now from various groups … showing excellent results, although longer follow-up is needed on all of these,” she said.
One such study is the GIMEMA ALL2820 trial looking at ponatinib plus blinatumomab vs imatinib plus chemotherapy, said Nicolas Boissel, MD, PhD, of Hôpital Saint-Louis in Paris, France, an invited discussant who addressed the European perspective on the PhALLCON results.
“It is expected that access to ponatinib will be delayed in Europe, compared with the US, so meanwhile, clinical trials remain a good option to give access to ponatinib frontline,” he said.
Going forward, Boissel said it will be important to determine the role of second-generation TKIs in patients who are ineligible to receive ponatinib, treatment duration needed to reduce the long-term risk of relapse, and the potential for eliminating the need for post-remission chemotherapy and stem cell transplantation in certain patients.
Advani added that, when evaluating and comparing treatments, it will be important to look at genomic alterations and BCR-ABL mutation status, age and comorbidities, and patterns of disease relapse, including relapse sites and genomics. Longer follow-up results for event-free survival and overall survival are also needed.
“I think, particularly in younger patients with relatively few or no cardiovascular comorbidities, [ponatinib plus reduced-intensity chemotherapy] represents a really exciting option,” Advani said. “What’s difficult is that the landscape is changing quickly in this field, and so is the standard of care. I think what we struggle with is whether we should be using antibody-based therapies plus TKIs or look at an approach such as this, and further studies are going to be needed to answer that question.”
Jabbour reported relationships with Pfizer, Takeda, Amgen, AbbVie, Bristol-Myers Squibb, Incyte, Adaptive Biotechnologies, Astellas Pharma, Genentech, and Ascentage Pharma Group. Luskin reported relationships with Pfizer, Novartis, and Abbvie. Advani reported relationships with Novartis, Glycomimetics, Kite Pharma, Seattle Genetics, Amgen, Beam Therapeutics, Mkarta, Taiho Oncology, Jazz Pharmaceuticals, Pfizer, and Kura Oncology. Boissel reported relationships with Amgen, ARIAD/Incyte, Novartis, SERVIER, and Astellas Pharma.
ASCO Plenary Series. February 15, 2023. Program Guide – ASCO Meeting Program Guide.
J Clin Onc. Published online February 17, 2023. Abstract. Study.
Sharon Worcester, MA, is an award-winning medical journalist based in Birmingham, Alabama, writing for Medscape, MDedge, and other affiliate sites. She currently covers oncology, but she has also written on a variety of other medical specialties and healthcare topics. She can be reached at [email protected] or on Twitter: @SW_MedReporter.
For more news, follow Medscape on Facebook, Twitter, Instagram, and YouTube.
Source: Read Full Article