SEATTLE — A family of blockbuster drugs for managing blood glucose — and now for promoting weight loss — has been linked to exacerbation of macular disease that frequently accompanies diabetes, new data show.
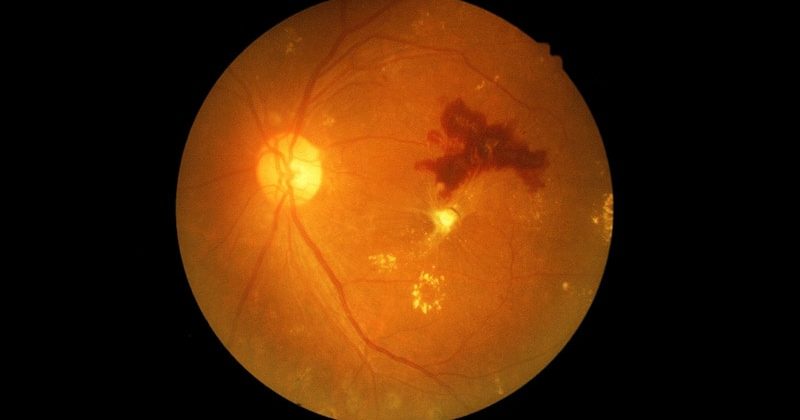
Two studies presented at the 2023 annual meeting of the American Society of Retina Specialists have found that use of injectable agonists of glucagon-like peptide-1 (GLP‑1) appears to hasten the progression of diabetic retinopathy and diabetic macular edema (DME).

Dr Ehsan Rahimy
Clinicians should be aware of these effects of GLP-1 inhibitors to ensure appropriate monitoring of patients for the possibility that retinopathy may accelerate, according to Ehsan Rahimy, MD, an adjunct clinical professor at Stanford University School of Medicine, Palo Alto, California, and colleagues.
Rahimy presented results of a retrospective study of retinopathy progression in patients taking either GLP-1 agonists or sodium-glucose transporter-2 (SGLT-2) inhibitors, also known as gliflozins. “When we looked at the conversion to proliferative disease, you can see it was statistically higher in the GLP-1 group at all timepoints,” he said.
GLP-1 agonists can promote considerable weight loss in patients with and without diabetes. Moreover, the finding that gliflozins improve cardiovascular and renal function in patients with type 2 diabetes has accelerated the use of these agents for blood glucose control.
Using a repository of data from more than 13,500 people taking either of the two kinds of medication, the researchers looked for conversion of diabetic eye disease to proliferative diabetic retinopathy (PDR) or DME. Secondary outcomes were the need for intravitreal injections, panretinal photocoagulation (PRP), or pars plana vitrectomy (PPV).
Propensity score matching for age, sex, race, ethnicity, and baseline A1c resulted in the inclusion of 5446 participants in each treatment group. After matching, the mean age of participants in either group was 64 years, and the mean A1c was 8.5%. Slightly more than half the participants were insulin-dependent.
Patients taking GLP-1 inhibitors had higher rates of conversion to PDR than those taking gliflozins at three years (6% vs 4%; P < .01), the researchers found. Nearly 25% of those taking a GLP-1 agonist had progressed to DME after 3 years, compared with 18% of those taking a gliflozin.
People in the group taking GLP-1 inhibitors also had a greater need for interventions than those on a gliflozin; 8% vs roughly 6%, respectively, required intravitreal injections, Rahimy reported. Similar trends were noted for need for PRP and PPV, he added, although the absolute numbers of patients were small.
Albiglutide the Key Culprit?
In other research reported at the meeting, a meta-analysis of data collected in 93 randomized clinical trials of the seven currently available GLP-1 agonists found only albiglutide was associated with diabetic retinopathy to a statistically significant degree. Compared with placebo, albiglutide more than doubled the risk for early-stage diabetic retinopathy (relative risk 2.18; 95% CI, 1.01 – 4.67; P = .05).

Ishani Kapoor
Other GLP-1 agonists evaluated in the meta-analysis included semaglutide, tirzepatide, dulaglutide, exenatide, liraglutide, and lixisenatide. These findings were reported in a poster presented at the meeting by Ishani Kapoor, MD Candidate, Drexel University College of Medicine in Philadelphia.
“The strength of these effects depends on the specific GLP-1 receptor agonist used, patient-specific clinical characteristics, and demographics,” Kapoor and co‑authors reported. “Further studies are needed to clarify the patient populations that would benefit from GLP-1 receptor agonists and those at risk for [the] development of additional ocular damage.”
What Causes Progression?
Whether worsening of retinopathy stems from rapid weight loss and acute reductions in concentrations of blood glucose or is a direct effect of GLP-1 agonists on the eye is unclear.
“That rapid reduction is thought to play some role,” Rahimy said. “But if you actually look out there in the basic science literature, it’s suggested that there are direct effects of these medications on the retina too. That being said, it’s suggested that they may be protective to the retina. And I think that’s where we’ve gotten a lot of mixed signals in our community between what we’ve seen on the basic science side vs what we’re seeing on the real-world side.”
The study was independently funded. Rahimy reports consultancies or speakerships with AbbVie, Allergan, Apellis, Carl Zeiss, Genentech, and Google and research support from Regeneron. Kapoor reports no relevant financial relationships.
2023 annual meeting of the American Society of Retina Specialists. Presented July 29–30, 2023.
Surv Ophthalmol. Published online July 16, 2023. Full text
A former staff reporter for Cardio magazine and contributor to MD Magazine’s vision disease coverage, Ellen Kurek earned her nonfiction writing certificate from the University of Washington.
For more news, follow Medscape on Facebook, Twitter, Instagram, YouTube, and LinkedIn
Source: Read Full Article