In a recent review published in Thrombosis Research, researchers reported the mechanisms involved in coronavirus disease 2019 (COVID-19) coagulopathy and the significance of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infections for cancer patients concerning outcomes, thromboembolic complication risks and consequences of management strategies.
Studies have reported that cancer patients are at an elevated risk of COVID-19 severity and associated adverse outcomes, either due to the neoplasm itself (such as lung cancers and hematological malignancies with hypercoagulable states) or due to immunological suppression as a result of antineoplastic therapy. Severe SARS-CoV-2 infections can be complicated by coagulopathies such as COVID-19, which can result in venous thromboembolism.
About the review
In the present review, researchers described COVID-19 coagulopathy pathways and their relevance in cancer patients concerning venous thromboembolic complications.
Mechanisms of COVID-19 coagulopathy
Severe COVID-19 has caused significant morbidity, including multiple organ dysfunction and respiratory insufficiency, and deaths. Age, obesity, and comorbidities such as hypertension, pulmonary disorders, and diabetes are established risk factors for COVID-19 severity. In addition, immunocompromised individuals such as those who received organ transplants, those on immunosuppressive medications, and those with hematological malignancies receiving anti-neoplastic agents, are highly prone to severe SARS-CoV-2 infections.
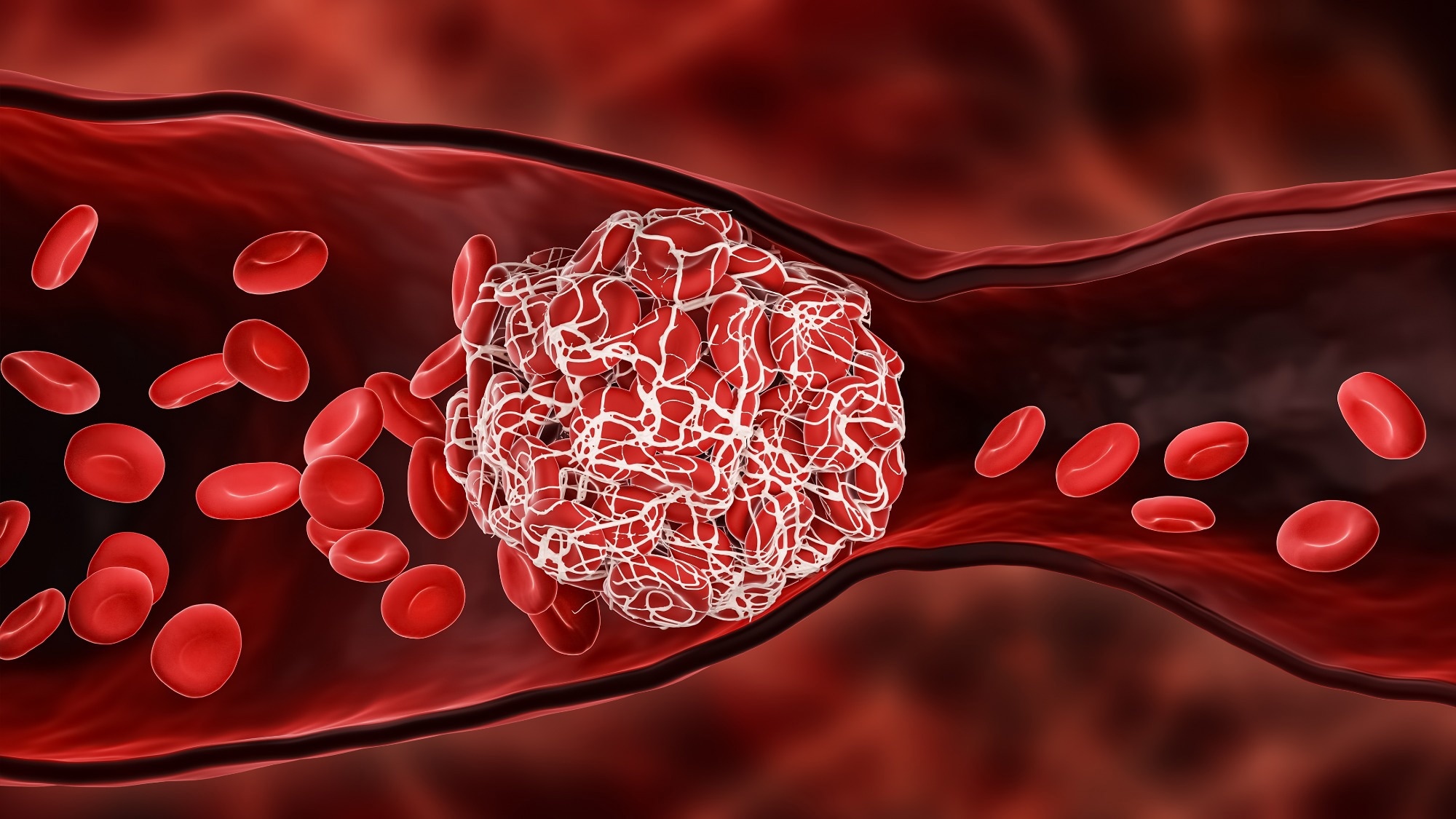
Severe COVID-19 patients develop hemostatic abnormalities such as venous thromboembolism, the risk for which is 12-fold higher among cancer patients than healthy individuals. SARS-CoV-2-associated coagulopathy is associated with significantly increased D-dimer levels with more profound elevations than those among cancer patients. In addition, serological levels of fibrinogen, factor VIII, and tissue-type plasminogen activators (t-PA) are elevated, in response to the cytokine storm [especially interleukin (IL)-6] in COVID-19, with abnormal coagulation and increased tissue viscoelasticity.
Elevated plasmin levels could activate metalloproteinase molecules in modifying extracellular matrices essential for leakage from capillaries and pulmonary edema. Platelet counts and coagulation inhibitors such as protein C and antithrombin are reduced in severe COVID-19. Further, SARS-CoV-2 infections are associated with neutrophil extracellular trap (NET) formation (NETosis) in blood vessels, induced by complement activation and IL-8.
NETs promote the formation of thrombus by activating the intrinsic clotting pathway and provide a platform for erythrocytes, platelets, and procoagulants like vWF (von Willebrand factor). Therefore, NETosis markers such as citrullinated histone H3 and myeloperoxidase (MPO)-deoxyribonucleic acid (DNA) complex are elevated in severe SARS-CoV-2 infections. NET-forming neutrophils co-populate with thrombocytes in COVID-19 patients’ pulmonary microthrombi, and NETs have been found in abundance in coronary vessel thrombi of COVID-19-associated myocardial infarction (MI) patients.
Perturbations in endothelial cells after vWF release provide an ideal surface for thrombus formation intravascularly in SARS-CoV-2 infections. ADAMTS13 (a disintegrin and metalloproteinase with a thrombospondin type 1 motif, member 13) cleaving capacity may be overwhelmed, resulting in thrombotic microangiopathies in the vessels of multiple organs in COVID-19. SARS-CoV-2 infection coagulopathy involving vessel wall thickening, stenosis, and microthrombi formation leads to a hypercoagulable situation, enhancing thromboembolic complication risks, potentiated by in-dwelling lines and immobilization among hospitalized SARS-CoV-2-positive patients.
Relevance of SARS-CoV-2-associated coagulopathy in cancer
Cancer patients with low lymphocyte counts, particularly those who underwent major surgeries or chemotherapy recently, have been reported to have two-fold and 1.2-fold higher COVID-19-associated mortality risks among hematological malignancy and other cancer patients. Studies have reported that coagulation and inflammatory responses to COVID-19 in cancer patients are greater than in non-cancer patients.
It has been documented that mild and severe COVID-19 patients have six-fold and three-fold higher risks of developing pulmonary embolism and venous thrombosis, respectively, the most prominent risk factor for which was the presence of active neoplasms. Venous thromboembolism has been reported to be higher (10%) among patients who received anti-neoplastic therapy in recent times compared to those who did not (six percent).
A growing body of evidence states that high-dose thrombosis prophylaxis has only marginally lesser safety and more efficacy in comparison to conventional dosage prophylaxis among hospitalized SARS-CoV-2-infected cancer patients; however, clinical research does not favor high-dose antithrombotic prophylaxis among severely ill COVID-19 patients, due to high bleeding risks. The finding could be extended to malignancy patients who also have elevated risks of bleeding.
Antithrombotic prophylaxis is not recommended for non-hospitalized malignancy patients who acquire SARS-CoV-2 infections; however, the risk-benefit ratio may tip towards conventional dose thrombosis prophylaxis for outpatients during active SARS-CoV-2 infections, but this needs to be confirmed in further clinical studies. Hematological malignancy patients have shown significantly lower seroconversion rates with low anti-SARS-CoV-2 antibody titers than healthy individuals. COVID-19 vaccines are considered safe for cancer patients, although there are concerns about messenger ribonucleic acid (mRNA) permeation and retention in tumor cells for mRNA vaccinations.
Overall, the review findings showed that COVID-19 could amplify the risk of venous thrombosis in active cancer patients, particularly among those on immunomodulators. Therefore, strategies for optimized protection of cancer patients against COVID-19 are essential. Management strategies to improve COVID-19 outcomes in malignancy patients (such as high-dose antithrombotic prophylaxis) are lacking and require further investigation with a focus on safety and efficacy.
- Marcel Levi, Nick van Es. (2022). COVID-19 associated coagulopathy and thrombosis in cancer. Thrombosis Research. doi: https://doi.org/10.1016/j.thromres.2021.12.006 https://www.thrombosisresearch.com/article/S0049-3848(21)00565-X/fulltext
Posted in: Medical Science News | Medical Research News | Disease/Infection News
Tags: Antibody, Bleeding, Blood, Blood Vessels, Cancer, Capillaries, Chemotherapy, Coronavirus, Coronavirus Disease COVID-19, covid-19, Cytokine, D-dimer, Diabetes, DNA, Edema, Efficacy, Embolism, Interleukin, Lymphocyte, Mortality, Myeloperoxidase, Myocardial Infarction, Neoplasm, Neutrophils, Obesity, Platelet, Platelets, Prophylaxis, Protein, Protein C, Pulmonary Edema, Pulmonary Embolism, Research, Respiratory, Ribonucleic Acid, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Stenosis, Syndrome, Thromboembolism, Thrombosis, Thrombus, Tumor, Venous Thromboembolism

Written by
Pooja Toshniwal Paharia
Dr. based clinical-radiological diagnosis and management of oral lesions and conditions and associated maxillofacial disorders.
Source: Read Full Article
