Severe inflammation in early childhood is a clinically known risk factor for developing autism and schizophrenia. Now, for the first time, scientists from the University of Maryland School of Medicine (UMSOM) have discovered that inflammation alters the development of vulnerable brain cells, and this could have mechanistic links to neurodevelopmental disorders. This finding could lead to treatments for many different childhood-onset neurodevelopmental disorders.
Using single-cell genomics to study the brains of children who died from inflammatory conditions—such as a bacterial or viral infections or asthma—along with those who died from a sudden accident, researchers from the University of Maryland School of Medicine led a study that found inflammation in early childhood prevents specific neurons in the cerebellum from maturing completely. The cerebellum is a brain region responsible for motor control and higher cognitive functions used in language, social skills, and emotional regulation.
Faculty from UMSOM’s Institute for Genome Sciences (IGS), Department of Pharmacology, and the University of Maryland-Medicine Institute of Neuroscience Discovery (UM-MIND) conducted the research.
The study appears in the October issue of Science Translational Medicine. It is part of a collection of nearly 30 papers describing the development and diversity of cell types in the human brain. All of these studies were coordinated by the Brain Research Through Advancing Innovative Neurotechnologies (BRAIN) Initiative Cell Census Network, a multisite consortium.
Previous research has shown that babies born with abnormalities of the cerebellum frequently go on to experience neurodevelopmental disorders, and animal models exposed to inflammation before birth also develop these conditions.
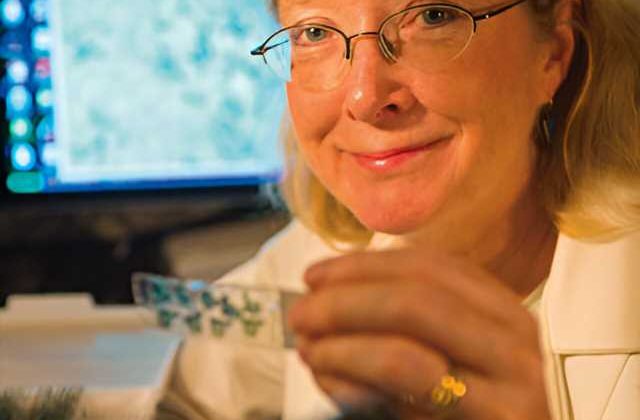
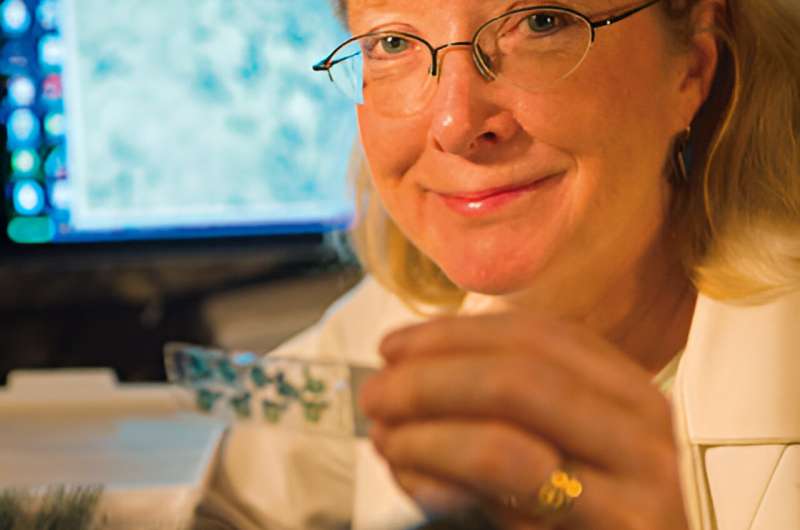
“We looked at the cerebellum because it is one of the first brain regions to begin developing and one of the last to reach its maturity, but it remains understudied,” said Seth Ament, Ph.D., IGS scientist and Associate Professor in the Department of Psychiatry at UMSOM who co-led the research with Margaret McCarthy, Ph.D., the James and Carolyn Frenkil Dean’s Professor and Chair in Pharmacology and Director of UM-MIND. “With the fairly new technology of single nucleus RNA sequencing we could look at the cell level to see changes in the brains.”
Dr. McCarthy added, “This has never been done before in this age group and in the context of inflammation. The gene expression in the cerebella of children with inflammation were remarkably consistent.”
The researchers examined donated post-mortem brain tissues of 17 children who died when they were one to five years old, eight from conditions that involved inflammation and nine from accidents. None of the donors had been diagnosed with a neurological disorder prior to death. The two groups were similar in age, gender, race/ethnicity, and time since death.
These unique brain tissue specimens had been collected over many years by UMSOM researchers at the University of Maryland Brain and Tissue Bank, the Maryland Brain Collection of the Maryland Psychiatric Research Center, and the NIH NeuroBioBank in Bethesda, Maryland.
The study found that two specific, yet rare types of cerebellar neurons were most vulnerable to brain inflammation—the Golgi and Purkinje neurons. At the single-cell level, these two types of neurons showed premature disruption of their maturation.
“Although rare, Purkinje and Golgi neurons have critical functions,” Dr. Ament said. “During development, Purkinje neurons form synapses connecting the cerebellum to other brain regions involved in cognition or emotional control, while Golgi neurons coordinate communication between cells within the cerebellum. Disruption of either of these developmental processes could explain how inflammation contributes to conditions like autism spectrum disorders and schizophrenia.”
As with many diseases, both genetics and the environment—in this case, inflammation—likely contribute to the risk of developing these disorders. That’s why it is crucial to understand the roles of specific cells within the brain regions—as well as how they interact with genes to influence brain function—to find treatments for brain disorders, like ASD and schizophrenia, as well as others including dementia, Parkinson’s disease, or substance use disorders.
“This study is one of the first to show that gene expression changes during inflammation may set the stage for later cellular dysfunction, such as reducing synaptic connectivity or altering energy metabolism,” said UMSOM Dean Mark Gladwin, M.D., who is also Executive Vice President for Medical Affairs, UM Baltimore, and the John Z. and Akiko K. Bowers Distinguished Professor at UMSOM.
“It’s critical to understand these mechanisms and changes at the cellular level during brain development in the hope that someday we can develop treatments for neurodevelopmental disorders.”
The data from this study—along with all of the BRAIN Initiative papers—has been deposited in the Neuroscience Multi-Omic Archive (NeMO Archive)—a curated genomic data repository—housed at the Institute for Genome Sciences at UMSOM. Neuroscience researchers can access the archive’s data through a user-friendly portal to transform their understanding of the complex workings of the brain.
More information:
Seth Ament et al, A single-cell genomic atlas for the postnatal maturation of the human cerebellum and the effects of early-childhood inflammation, Science Translational Medicine (2023). DOI: 10.1126/scitranslmed.ade1283. www.science.org/doi/10.1126/scitranslmed.ade1283
Journal information:
Science Translational Medicine
Source: Read Full Article