
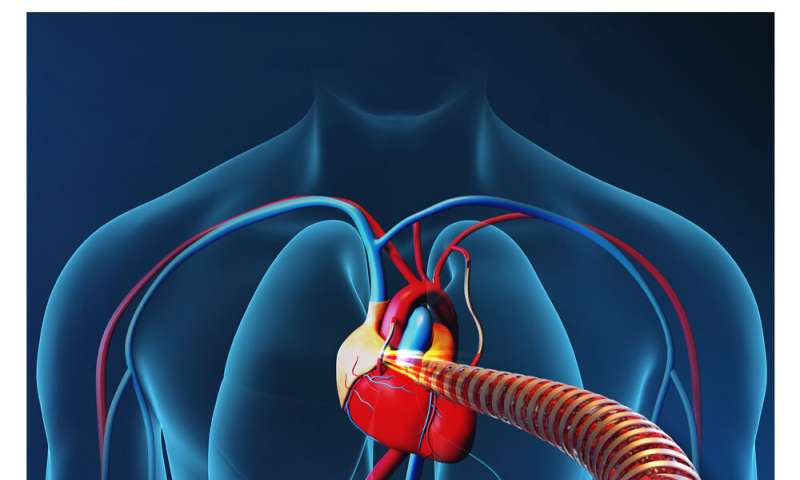
Researchers in China and Switzerland have developed electronic blood vessels that can be actively tuned to address subtle changes in the body after implantation. The blood vessels—made of a metal-polymer conductor membrane that’s flexible and biodegradable—mimic natural blood vessels, were conductive in in vitro experiments, and were able to effectively replace key arteries in rabbits. The research, published October 1 in the journal Matter, could overcome the limitations of conventional tissue engineered blood vessels (TEBVs), which serve as passive scaffolds, by coordinating with other electronic devices to deliver genetic material, enable controlled drug release, and facilitate the formation of new endothelial blood vessel tissue.
“We take the natural blood vessel-mimicking structure and go beyond it by integrating more comprehensive electrical functions that are able to provide further treatments, such as gene therapy and electrical stimulation,” says lead author Xingyu Jiang, a researcher at Southern University of Science and Technology and the National Center for NanoScience and Technology in China.
Previous research has developed a variety of TEBVs that provide mechanical support for hard-to-treat blockages of tiny blood vessels in patients with cardiovascular disease. But these TEBVs have limitations: they cannot proactively assist in regenerating blood vessel tissue and, unlike natural tissue, often cause inflammation in response to blood flow. “None of the existing small-diameter TEBVs has met the demands of treating cardiovascular diseases,” says Jiang.
To surpass the limitations of existing technologies, Jiang and colleagues fabricated biodegradable electronic blood vessels using a cylindrical rod to roll up a metal-polymer conductor membrane made from poly(L-lactide-co-ε-caprolactone). They showed that, in the lab, electrical stimulation from the blood vessel increased the proliferation and migration of endothelial cells in a wound healing model, suggesting that electrical stimulation could facilitate the formation of new endothelial blood vessel tissue. The researchers also integrated the blood vessels’ flexible circuitry with an electroporation device, which applies an electrical field to make cell membranes more permeable, and observed that the combined technologies successfully delivered green fluorescent protein DNA into three kinds of blood vessel cells in the lab.
Next, the researchers tested the device in New Zealand rabbits, replacing their carotid arteries—which supply blood to the brain, neck, and face—with electronic blood vessels. Jiang and colleagues monitored the implants using doppler ultrasound imaging over the course of three months, finding that the device allowed for sufficient blood flow the entire duration. Imaging tests that use X-rays and dye to peer inside arteries revealed that the artificial arteries appeared to function just as well as the natural ones had, with no sign of narrowing. When the researchers removed the implants and analyzed the rabbits’ internal organs at the end of the three-month period, they discovered no evidence that the devices had produced an inflammatory response.
While these electronic blood vessels demonstrated promise as surrogate arteries in rabbits, Jiang acknowledges that more work must be done before the technology will be ready for human trials, including long-term safety tests in larger cohorts of rabbits and other animals. Additionally, in order to be suitable for long-term implantation, the electronic blood vessels would need to be paired with smaller electronics than the electroporation device used in this study.
Source: Read Full Article
