People who do not live in early hit cities may be at greatest risk during a second wave of COVID-19, according to new research from scientists at the University of Sussex and the Francis Crick Institute.
Their research tracks the daily COVID-19 death rates in major cities (London, New York, Madrid and Milan/Lombardy) of four hard-hit countries, and compares it with the corresponding nations as a whole.
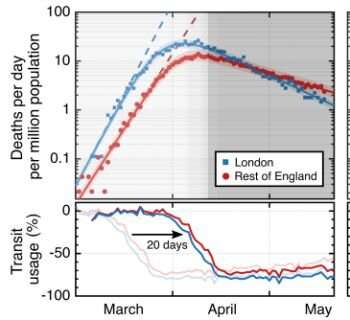
They show that after lockdown—and indeed slightly before lockdown—death rates slowed more quickly in these early hit cities than in the rest of the population. The researchers conclude this is because coronavirus infection became more widespread in these main metropolitan regions, with the result that fewer people remained susceptible to infection and therefore COVID-19 was less able to spread.
The findings show that, for all four countries, the number of people remaining susceptible to the disease has been reduced more in early hit cities due to the disease being seeded sooner there. In spite of the heavy death toll in these cities, this difference in remaining susceptibility means that the other areas of each country would need to brace for a higher per capita death rate in the event of a second wave. Of the cities studied, this effect is particularly large in London.
The research also indicates that more people have had COVID-19 than we previously realized—these results are derived from the disease dynamics analysis rather than serology testing for antibodies or live infections, which are both prone to selection bias, under-representative population sampling and insufficient reliability.
The data shows that as many as 45% of Londoners could have been infected, compared to just under 20% for the rest of the country. In New York the findings reveal that 41% of the population could have had the infection, compared to only 5% of the rest of the U.S..
Professor Peter Krüger, a physicist and data scientist at the University of Sussex, said:
“Our research compared daily death rates in London versus England as a whole, Madrid versus Spain, Lombardy versus Italy and New York versus the US. We show that in these cities, the death rate dropped more steeply than elsewhere after lockdown started. That is because in these early hit cities, the spread of coronavirus infection was already beginning to slow due to fewer people remaining susceptible. In effect, it is as if lockdown was introduced later in the cities than in the rest of their respective countries because the pandemic had reached a more advanced stage there. Taking the example of the UK, our research shows that had the UK government continued the lockdown period for longer, we could now have entered a containable situation, with infection rates lower than ten people per million. Combined with a working track and trace system, things could have been quite different. Instead, the UK is in a halfway house—where the disease was allowed to spread out of control but was also never brought fully back under control before lockdown was eased. Infection rates in England are still well above containment level, with a large number of people who remain at risk of infection. What’s more, a recent study commissioned by [Government Chief Scientific Adviser] Patrick Vallance found that a second wave could be more deadly than the first. Our analysis indicates that this may be most true outside of the initially hard-hit cities. In contrast to previously published models, which do not factor in the effect of waning population susceptibility, our data suggest that projections which accommodate the effect of widespread exposure provide more granular, and likely more accurate, information. The relaxation of distancing measures has slowed the decline in death rates. The UK government is aiming to keep the R rate just below 1, but this is not enough to contain the disease any time soon. In fact, our results show that if we did not have the reduction of susceptibility that we have now, then with current easing of lockdown, we would not be seeing a decline in death rates but an increase instead. We also find that the recent slowdown of the decline in daily death rates in England clearly correlates with the lifting of lockdown. This slowdown in their decline is an important and potentially ominous trend; our findings indicate a need for close following of the numbers in coming months.”
Dr. Karen Patterson, who is co-lead author on the study and an expert in respiratory medicine and critical care at Brighton and Sussex Medical School and the Francis Crick Institute, said:
“Not only do the non-early hit areas have the largest proportion of people who have yet to be infected, and therefore do not have immunity, these areas also have fewer critical care beds per capita. For the case of England, should a second wave occur, our results serve as an alarm bell for the non-London areas to be especially well prepared. Given the high death counts seen in London in the spring, it may be counter-intuitive to consider that the infection fatality rate appears actually to be lower in London compared to the rest of England. We found that the infection fatality rate is approximately 35% smaller in London compared to elsewhere in England. This is an effect of people in London being younger. In addition, Londoners on average have lower rates of key health conditions which impact outcomes in COVID-19. As an additional consideration, the increased vulnerability of areas outside the early hit cities has implications for vaccine trial planning, where the larger population susceptibility found outside the early hit cities may better serve these trials. If you want to test if a vaccine works, you cannot trial it on an immune population.”
Source: Read Full Article
